Gotcha thanks
B/CS number of cases update? 11-17-20 Staff Edit on OP
1,194,394 Views |
6626 Replies |
Last: 2 yr ago by Nosmo
You really should just quit posting on this thread. Or give your name and credentials to substantiate your posts.
This is an false statement. Heart attacks, strokes, pneumonia, car accidents, trauma, non-swimmers in the water at Lake Bryan, very very medically ill individuals.Quote:
Normally ICUs are not busy in the summer
The ICU at St Joseph's is busy all 12 months of the year pre-Covid.
Thank you posting this article.lockett93 said:
https://medium.com/analyticaper/covid-19-what-the-data-tells-us-3a08e42ee36f
Good article...
Quote:
First, let me give you a SUPER high level summary:
- Covid19 is serious, but it's significantly less than we thought
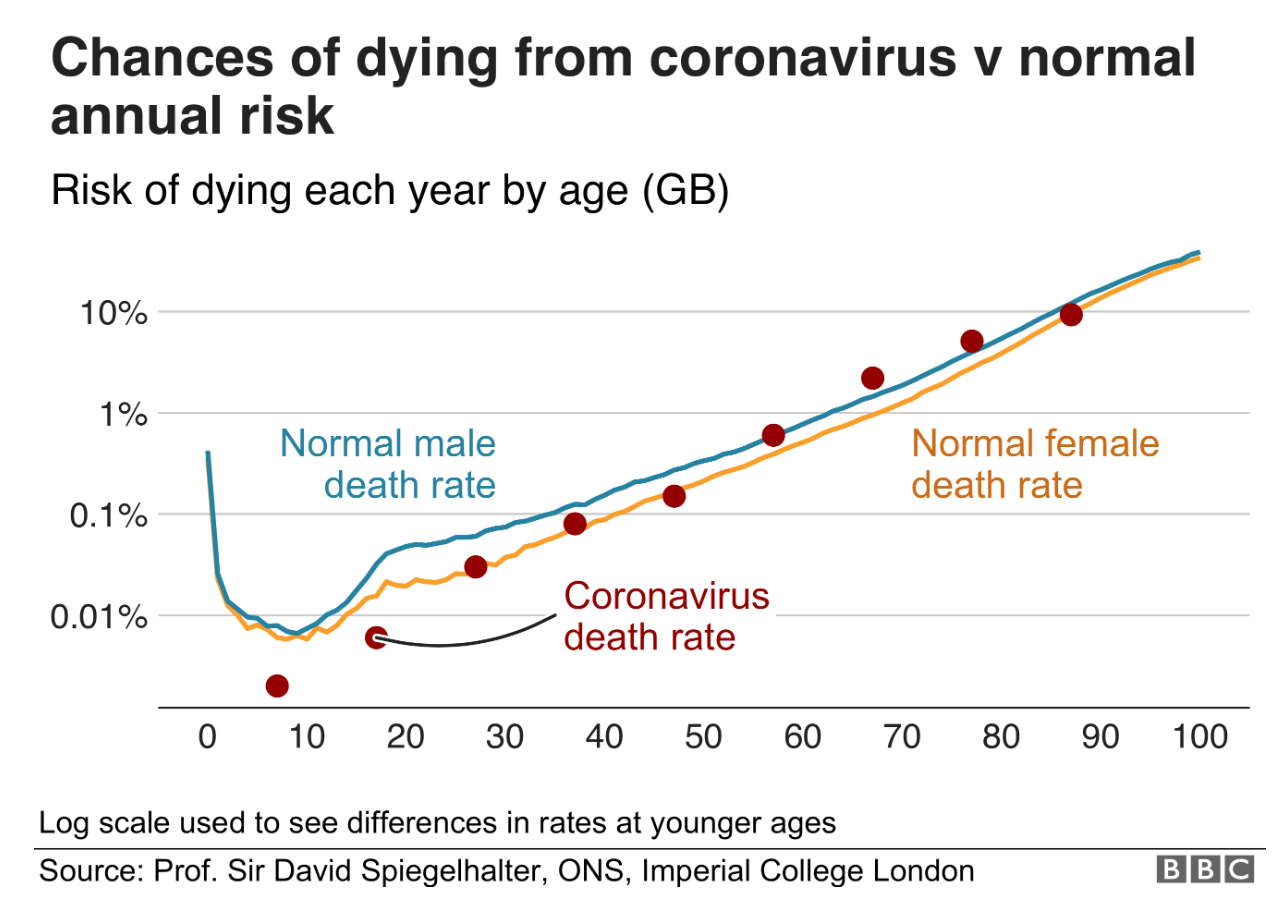
- Fatality: According to data from the best-studied countries and regions, the lethality of Covid19 is on average about 0.3%, which is about ten times lower than originally assumed by the WHO. As of 5/20/2020 the CDC is now estimating ~0.26% in the U.S.
- Fatality in Context (i.e. Risk): The risk of death for the general population of school and working age is typically in the range of a daily car ride to work. The risk was initially overestimated because many people with only mild or no symptoms were not taken into account. i.e. we're capturing most of the deaths but only 510% of the infections. Risk varies by age significantly. For kids (particularly toddlers), they are ~20X's more likely to die from the Flu or Pneumonia than Covid. For those over age 70, the risk of fatality is ~2.5% this is much higher for those in poor health.
Harris County (total) has a base line capacity of 1,622 ICU beds, of which 93% are occupied, with 29% COVID-only. There are about ~100 ICU beds left in the county, with an ability to swell the ICU bed count by ~20% (325 beds) for surge capacity.Rapier108 said:No they won't.musicforall said:
When Houston ICU beds fill up, will they be sent here? Just curious.
Brazos County already has to cover multiple surrounding counties.
Second, Houston is no where close to having its ICU beds full. The TMC is not the only hospital in Houston, but their numbers, which are no where near full (ICU is around 28% virus patients, the rest are for other things) but often reported as representing all of Houston, do not represent all of the hospitals outside of the TMC, and in surrounding areas.
By comparison, the TMC includes 1,330 ICU beds, or about 82% of Harris County's total. TMC hit 100% ICU beds yesterday (reported today), and is probably working into the surge capacity (which they're totally prepared for, but less than ideal).
But to the original question, Houston will receive patients from outlying areas -- not redirect them into outlying hospitals. Here's hoping the surge capacity stands up, otherwise they'll start overtaking general admission beds (again, contingency plans in-place for but less than ideal).
source?ToxicAG said:
There is also staffing issues, since an ICU patient takes more care than normal patients.
Well, if they didn't, they wouldn't be in ICU.
ICU staff to patient ratio is either 1:1 or 1:2. A "regular" hospital unit might be as much as 1:10.
If they are vented, you also need additional respiratory therapists available.
You also typically have an aide for every 4 patients instead of 2-3 for an entire floor.
Source: I'm a retired critical care RN.
ICU staff to patient ratio is either 1:1 or 1:2. A "regular" hospital unit might be as much as 1:10.
If they are vented, you also need additional respiratory therapists available.
You also typically have an aide for every 4 patients instead of 2-3 for an entire floor.
Source: I'm a retired critical care RN.
I work in the cancer field and normal nurse staffing can fluctuate from 1:5/10 per nurse. For ICU patients it is at 1:1 to 1:2 with special training.
Ribbed Paultz said:
Where are you getting that statistic of only 27% of ICU patients are COVID-19 patients in the TMC?
If true, that is stunning to me. Normally ICUs are not busy in the summer. So if not COVID-19 patients, why are the ICUs so full?
I'm not sure why this is stunning to you. Hospitals don't build huge ICU wards expecting them to be empty. That would be a good way to go broke.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3840149/
The above 2013 study showed over a 3 year period that ICU occupancy ranged from 57.4% to 82.1%, with mean hourly occupancy of 68.2%.
Table 1 on the second page of the following article shows that the larger a hospital is, the higher its overall average occupancy is. Note the percentages for large hospitals (82.5% for hospitals with 500 or more beds, 81.7% for hospitals with 400-499 beds):
https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/HealthCareFinancingReview/Downloads/CMS1191873dl.pdf
In other words, current levels of hospital occupancy aren't terribly unusual.
I have talked to colleagues (oncologists) about this and there is worry is that the level care will decline with the increase in ICU beds due to staffing. What are your thoughts?trouble said:
Well, if they didn't, they wouldn't be in ICU.
ICU staff to patient ratio is either 1:1 or 1:2. A "regular" hospital unit might be as much as 1:10.
If they are vented, you also need additional respiratory therapists available.
You also typically have an aide for every 4 patients instead of 2-3 for an entire floor.
Source: I'm a retired critical care RN.
Are these sources good enough for you?
jim james
It's always possible but I wouldn't expect it.
https://ktrh.iheart.com/content/2020-06-25-houston-hospital-leaders-say-they-have-bed-capacity-in-case-of-covid-surge/
Straight from the hospitals themselves. I'll defer to them as to wether fear is warranted. They have contingency plans, the plan for emergencies, overflow, etc.. 100% does not mean that's it and their done in this case. It's based on normal operating capacities, from all sources, wether COVID, elective or emergency procedures. By pushing back electives, bed space will be freed up.
Hopefully they can find a balance as to not cause money shortages again with few patients and surgical procedures which pay the bills.
Straight from the hospitals themselves. I'll defer to them as to wether fear is warranted. They have contingency plans, the plan for emergencies, overflow, etc.. 100% does not mean that's it and their done in this case. It's based on normal operating capacities, from all sources, wether COVID, elective or emergency procedures. By pushing back electives, bed space will be freed up.
Hopefully they can find a balance as to not cause money shortages again with few patients and surgical procedures which pay the bills.
trouble said:
Well, if they didn't, they wouldn't be in ICU.
ICU staff to patient ratio is either 1:1 or 1:2. A "regular" hospital unit might be as much as 1:10.
If they are vented, you also need additional respiratory therapists available.
You also typically have an aide for every 4 patients instead of 2-3 for an entire floor.
Source: I'm a retired critical care RN.
Trouble, not arguing that or your bona fides.
I meant a source that there is a shortage of staff.
jwj said:
Are these sources good enough for you?
No. Toxic still hasn't demonstrated a staff shortage, only his/her personal opinion/concern.
I don't dispute the credibility of Trouble or Toxic's expertise in their fields.
I'm sure both are fine Health Care professionals.
That doesn't mean there is a staff shortage.
I'll let them clarify, but I got the impression that they are concerned that there could be a shortage of skilled staff to care for ICU patients if the hospitals are overwhelmed beyond the current surge projections and planning. Caring for multiple patients on ventilators requiring heavy sedation/paralysis, dialysis, pressors for blood pressure support, ECMO, etc will require skilled medical personnel 24/7. Sustaining that level of care could be difficult for some hospital systems in some areas. In Texas, I don't think we are at this point yet. And I hope we never get there.Quote:
That doesn't mean there is a staff shortage.
The nursing shortage has can pretty well documented for a while. There's a finite number of ICU nurses. You can't just pull someone from another floor and have them take ICU patients.
OK. My hesitation here is, and this is not pointed at you personally as you've brought some very thoughtful insight into this discussion, this seems to be another instance of "moving the goalposts."
We've gone from ventilators, to tests, to ICU beds, and now skilled nurses.
It seems that every time one conundrum is addressed a new crisis is on the horizon and yet another reason for panic and hysteria (by some).
We've gone from ventilators, to tests, to ICU beds, and now skilled nurses.
It seems that every time one conundrum is addressed a new crisis is on the horizon and yet another reason for panic and hysteria (by some).
Most medical professionals will tell you that summers are not as busy as winters on hospital inpatient floors and ICUs.
That's supported by this study from 2010- https://pubmed.ncbi.nlm.nih.gov/20156706/
So yes, it is stunning that the hospitals and ICUs are approaching capacity in the summer when it's not COVID-19 patients that are filling them up.
It makes me wonder if people aren't seeking care for other conditions before they get to the point of needing hospital/ICU admission. Or maybe the increased stress and economic hardship of the pandemic is contributing.
That's supported by this study from 2010- https://pubmed.ncbi.nlm.nih.gov/20156706/
Quote:
During the study period, 3,115 patients, coming from the Emergency Department, were hospitalized in our ICU. Of these, 21% were admitted during the summer, an incidence rate that is statistically lower than in other seasons of the year (P<0.001).
So yes, it is stunning that the hospitals and ICUs are approaching capacity in the summer when it's not COVID-19 patients that are filling them up.
It makes me wonder if people aren't seeking care for other conditions before they get to the point of needing hospital/ICU admission. Or maybe the increased stress and economic hardship of the pandemic is contributing.
You're citing an 11-yr-old article from data from a hospital in the Canary Islands???
The title is "Seasonal Influence in Characteristics of Patients Admitted to an Intensive Care Unit" and the conclusion is "The stability of our climate implies that this factor does not influence the prognosis of patients who are admitted with critical illness."
While the abstract is in English, the entire article is in Spanish. Therefore, I can't evaluate the entire article.
Apples and Oranges.
The title is "Seasonal Influence in Characteristics of Patients Admitted to an Intensive Care Unit" and the conclusion is "The stability of our climate implies that this factor does not influence the prognosis of patients who are admitted with critical illness."
While the abstract is in English, the entire article is in Spanish. Therefore, I can't evaluate the entire article.
Apples and Oranges.
For me, ICU beds and nurses were always connected. Just like respiratory therapists and ventilators. When they talked months back about ramping up production of vents, I asked who was going to be available to monitor all these ventilated patients.
Again, it totally depends on the hospital. Trauma centers are busy year round.
That was such a bizarre time during all this. Turns out we didn't need the extra ventilators. But if we did it would've resulted in an all hands on deck situation. Maybe pulling medical students/residents into running the vents?
They would not have sufficient training or experience. Running a vent on a critical patient cannot be left in the hands of a medical student or surgery/internal med/derm/radiology/etc resident.Quote:
Maybe pulling medical students/residents into running the vents?
Lord help us all
please explain. Truly curious and I have no frame of reference. What makes ventilators so hard?MiMi said:They would not have sufficient training or experience. Running a vent on a critical patient cannot be left in the hands of a medical student or surgery/internal med/derm/radiology/etc resident.Quote:
Maybe pulling medical students/residents into running the vents?
IMO you could train a med student or resident to manage a vent in a fairly short frame of time if that was all they had to do. I know in residency I was managing NICU vents & PICU vents with marginal oversight from RT/Attendings @ TCH.MiMi said:They would not have sufficient training or experience. Running a vent on a critical patient cannot be left in the hands of a medical student or surgery/internal med/derm/radiology/etc resident.Quote:
Maybe pulling medical students/residents into running the vents?
Now managing multiple drips, hanging drips, adjusting rates-- basically asking them to be RT & RN -- would take a good while.
As competitive as derm is to get into those residents could learn to manage a vent very quickly. Super smart folks.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
I'll try....pretend your job is to monitor all the traffic lights in a major city. No problem! The computer in front of you handles it all automatically. You know where the on/off switch is, but that's about it. An alarm goes off! What is that? What does it mean? Is it serious? What do I need to adjust to correct it? Is it something I'm qualified to change or do I need my supervisor to step in? Wait, that one cleared up on its own, but now there's a wreak at a major intersection! How can I best reroute/fix the problem? Do I even know how to fix it?cavscout96 said:please explain. Truly curious and I have no frame of reference. What makes ventilators so hard?MiMi said:They would not have sufficient training or experience. Running a vent on a critical patient cannot be left in the hands of a medical student or surgery/internal med/derm/radiology/etc resident.Quote:
Maybe pulling medical students/residents into running the vents?
There are a lot of moving parts to the whole ventilation thing. It's complicated and requires skill and experience to manage it well.
It's "easy" to say, we can put in place more beds, more ventilators, more monitors, more pumps, etc., but without the proper personnel, you can't really run an ICU.
Ventilators used for COVID patients have more than an on/off switch. The user must have a solid understanding of respiratory physiology and be able to know how and when to adjust certain parameters, such as tidal volume, minute ventilation, Fi02, PIP, and PEEP (just to name a few). Ask an orthopedic surgeon to interpret an arterial blood gas sample or a capnography waveform and tell you what is abnormal and how to correct it by altering the ventilator settings.Quote:
What makes ventilators so hard?
A seasoned Ortho I agree because it has been years or decades since they recalled that information- an ortho resident is very likely to remember all of that as they just had to ace a test about it in order to get into residency.MiMi said:Ventilators used for COVID patients have more than an on/off switch. The user must have a solid understanding of respiratory physiology and be able to know how and when to adjust certain parameters, such as tidal volume, minute ventilation, Fi02, PIP, and PEEP (just to name a few). Ask an orthopedic surgeon to interpret an arterial blood gas sample or a capnography waveform and tell you what is abnormal and how to correct it by altering the ventilator settings.Quote:
What makes ventilators so hard?
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
I don't know. I used to take a week off in June just to prepare for July 1.
Yes because medical students are taught and expected to know EVERYTHING. That is why they spend 3+ years in residency focusing on a specific field after medical school. They are very smart young people though and if you wanted them to hyperfocus on vent care they could master it in quickly. This is from my experiences of teaching these students for the last 5 years.trouble said:
I don't know. I used to take a week off in June just to prepare for July 1.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.



