Post Reply
1 of 1
For the Docs - Blood Clot conversation
3,134 Views |
22 Replies |
Last: 4 yr ago by Pelayo
I agree with everything except "most" deaths being due to clots. We are finding more DVTs in these patients than would normally be expected, and anything with this degree of systemic inflammation is going to be very pro-thrombotic, but the leading causes of death are pretty clearly refractory hypoxia from ARDS and left heart failure likely due to myocarditis. I'm sure a bunch of these patients have pulmonary emboli as well and done may very well be coding from massive PEs but I can't support the claim that it's likely a huge percentage of those dying.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
Agree. "Many, maybe most clots causing death." Is she actually seeing these pts? Witnessing the cytokine storm? Scary to me that nationally respected Drs getting on social media and making the baseless claims. She's a breast oncologist.
Yeah, if you're not in pulm/crit, EM, ID, cardiology or a COVID specific hospitalist service you almost certainly haven't seen enough of these patients to have a good feel for the course of the disease. That's a knock on other fields either, I sure as hell can't treat breast cancer. It's all about volume of exposure.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
I might include nephrology in that group as well, a lot of these folks are requiring CRRT and advanced avid/base management.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
Appreciate the responses.
I'm Heme/Onc and I don't THINK what she thinks is true. I have not seen a COVID pt but I see clots ALL the time. That's what Heme does. 

No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
Not dissecting the original tweet but find the suggestion of hypercoagulability interesting. Have seen a patient that required TPA for presumed PE. Dvt was verified.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
Yes the irony. Today lost one to a huge PE. Covid pos. Probably something to this. But I don't think it's the main mechanism of these patients dying.
I've been thinking about this a lot lately. It would explain the profound hypoxia without the presence of ARDS at least in some patients initially with good lung compliance. I've also seen some theories regarding it creating a functional hemoglobinopathy affecting oxygen delivery. Not sure how we could increase oxygen delivery, however. Have you all been getting TEGs on these patients?
https://chemrxiv.org/articles/COVID-19_Disease_ORF8_and_Surface_Glycoprotein_Inhibit_Heme_Metabolism_by_Binding_to_Porphyrin/11938173
https://chemrxiv.org/articles/COVID-19_Disease_ORF8_and_Surface_Glycoprotein_Inhibit_Heme_Metabolism_by_Binding_to_Porphyrin/11938173
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
watch, now everyone with a cough will get a CTAPikesPeakAg said:
Not dissecting the original tweet but find the suggestion of hypercoagulability interesting. Have seen a patient that required TPA for presumed PE. Dvt was verified.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
When it comes to coronavirus, I've wondered about my dad who's Factor V Leiden has always led to secondary complications when he's had health issues, would come into play.
As a radiologist, I wondered if that ever stopped.Pelayo said:watch, now everyone with a cough will get a CTAPikesPeakAg said:
Not dissecting the original tweet but find the suggestion of hypercoagulability interesting. Have seen a patient that required TPA for presumed PE. Dvt was verified.
Ha!jac4 said:As a radiologist, I wondered if that ever stopped.Pelayo said:watch, now everyone with a cough will get a CTAPikesPeakAg said:
Not dissecting the original tweet but find the suggestion of hypercoagulability interesting. Have seen a patient that required TPA for presumed PE. Dvt was verified.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
We have observed an awful lot of thrombotic complications in patients with COVID19 who are critically ill in our ICUs: clotted central lines and dialysis catheters, clotted dialysis filters, DVTs/PTEs, strokes. We've also observed a high rate of acute renal failure in normotensive patients and a few cases of sudden, unexplained cardiomyopathy which have led us to speculate about microthrombi. Not able to put it all together yet but participating in a 2-hour teleconference about this tomorrow morning with experts in thromboembolic disease from around the country.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
Agree 100%. I am sure the risk of DVT is higher in patients given the high cytokine storm, thus why their CRPs are through the roof....however I doubt this is the major cause of death. I still believe ARDS and shock are the major causes.....not a large saddle PE. I would assume 40mg lovenox sq qd, would be sufficient, however obviously we are still learning things by the day. There has been some autopsys that show covid can cause endothelial myocardial sloughing---->microvascular occlusion, thus higher anticoagulation may be beneficial? Still, so much to learn.Infection_Ag11 said:
I agree with everything except "most" deaths being due to clots. We are finding more DVTs in these patients than would normally be expected, and anything with this degree of systemic inflammation is going to be very pro-thrombotic, but the leading causes of death are pretty clearly refractory hypoxia from ARDS and left heart failure likely due to myocarditis. I'm sure a bunch of these patients have pulmonary emboli as well and done may very well be coding from massive PEs but I can't support the claim that it's likely a huge percentage of those dying.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
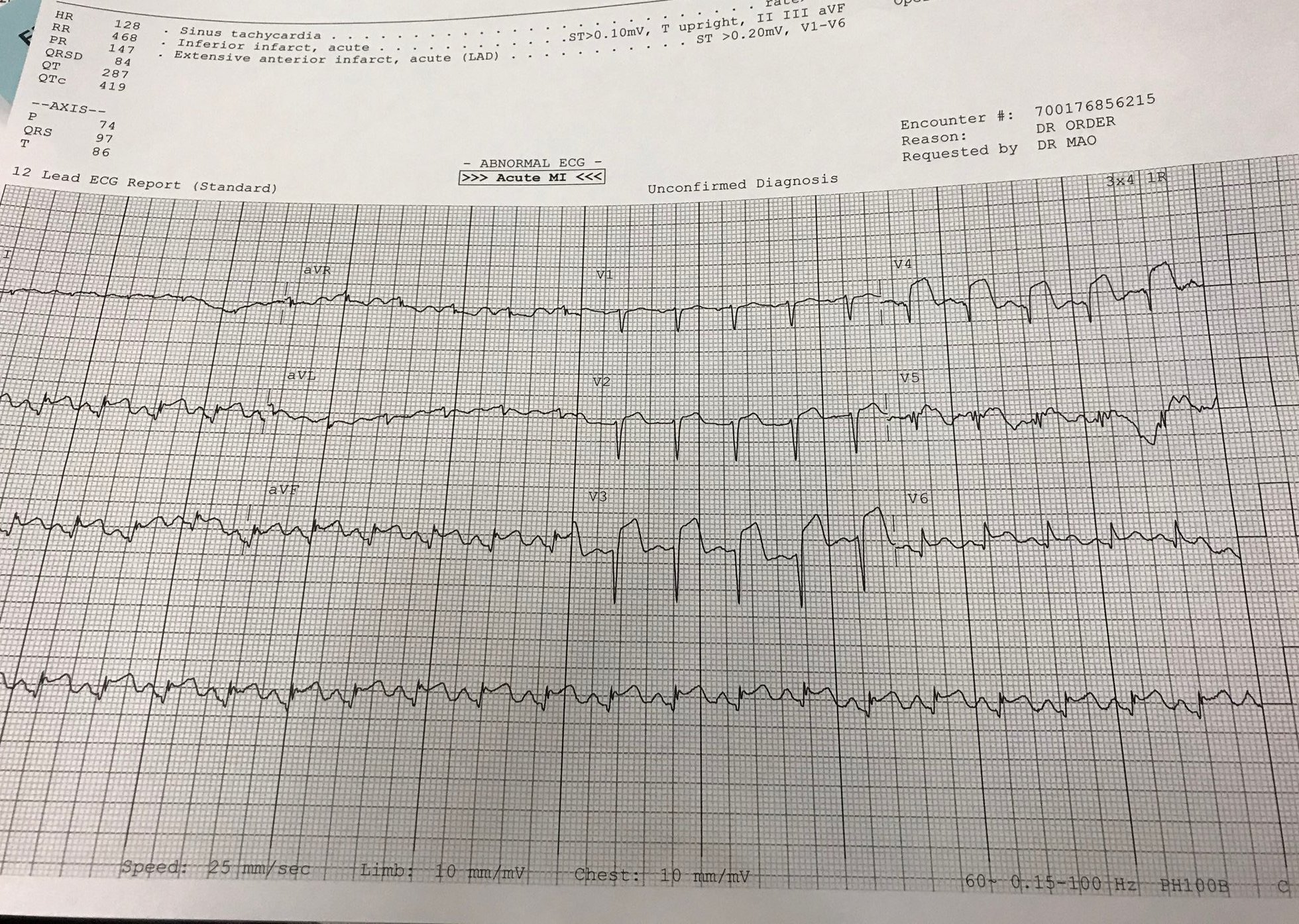
For the ER docs and cards out there. EF 40%, covid +, mild CAD
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
Just curious about patient's clinical course if you don't mind sharing.... COVID + pt whom also was found to have PE early on, or a patient covid + whom deteriorated later in the ICU? In the ER we are seeing a lot of covid + pts, and to be honest we are trying to avoid CT when possible because each covid + patient then requires an hour long clean in the scanner afterwards. Begs the question, should hypotensive covid + patients just get full dose tpa if they are on the brink of coding? Treat like a massive PE.Marcus Aurelius said:
Yes the irony. Today lost one to a huge PE. Covid pos. Probably something to this. But I don't think it's the main mechanism of these patients dying.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
She was admitted for worsened MS symptoms 3/9. Contracted COID nosocomial. Disturbing.
damn
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
Doug Ross said:
For the ER docs and cards out there. EF 40%, covid +, mild CAD
Every time I think I miss my general medicine days in residency I see something like this, remember the 2 AM sphincter puckering and suddenly I'm good again.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
Wow. Are you saying the cath showed mild cad or he had a history of mild cad when he presented?Doug Ross said:
For the ER docs and cards out there. EF 40%, covid +, mild CAD
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
It does. Tough without more data.Quote:
Begs the question, should hypotensive covid + patients just get full dose tpa if they are on the brink of coding? Treat like a massive PE.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
I can honestly say I don't miss much of anything about residency, and it's been two decades. Fellowship was another story.Infection_Ag11 said:Doug Ross said:
For the ER docs and cards out there. EF 40%, covid +, mild CAD
Every time I think I miss my general medicine days in residency I see something like this, remember the 2 AM sphincter puckering and suddenly I'm good again.
No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. See full Medical Disclaimer.
Featured Stories
See All
Elko: RB Moss out for remainder of 2024 season due to injury
by Olin Buchanan
No. 13 Texas A&M shocked by UCF in season-opening upset, 64-61
by Luke Evangelist
2026 Fairburn (GA) Langston Hughes TE Xavier Tiller commits to Texas A&M
by Ryan Brauninger
6:11
3h ago
706
54:39
12h ago
2.8k



