ttu_85 said:
I'm but a lowly tard with a CS background. We too have our own unique terminology, acronym etc. I understand the OP was rushed and had to use his instinctive terminology to get this out to the masses with the time available to him.
This document critically important and the best I have heard anywhere regarding this crisis. If any medical professional could edit it for the medical layman that would be so helpful.
God bless the OP for taking the time to share this critical information and for their work in the trenches.
Notes added in parenthesis for the layperson. Please let me know if I misinterpreted anything.
I just spent an hour typing a long post that erased when I went to change the title so I apologize to the grammar and spelling police. This one will not be proofread and much shorter.
I am an ER MD in New Orleans. Class of 98. Every one of my colleagues have now seen several hundred Covid 19 patients and this is what I think I know.
Clinical course is predictable.
2-11 days after exposure (day 5 on average) flu like symptoms start. Common are fever, headache, dry cough, myalgias (
general muscular pain; back pain indicated as common), nausea without vomiting, abdominal discomfort with some diarrhea, loss of smell, anorexia, fatigue.
Day 5 of symptoms- increased SOB (
shortness of breath), and bilateral viral pneumonia
(double pneumonia) from direct viral damage to lung parenchyma (
the portion of the lung involved in gas transfer - the alveoli, alveolar ducts and respiratory bronchioles.) Day 10- Cytokine storm (
overproduction of immune cells and their activating compounds (cytokines), signaling an inflammatory response flaring out of control) leading to acute ARDS (
Acute respiratory distress syndrome) and multiorgan failure. You can literally watch it happen in a matter of hours.
81% mild symptoms, 14% severe symptoms requiring hospitalization, 5% critical.
Patient presentation is varied. Patients are coming in hypoxic (
poor oxygen saturation; below 90%) even 75% without dyspnea (
labored breathing). I have seen Covid patients present with encephalopathy (
brain injury, headache), renal (
kidney) failure from dehydration, DKA (
Diabetic ketoacidosis: occurs when the body starts breaking down fat at a rate that is much too fast. The liver processes the fat into a fuel called ketones, which causes the blood to become acidic). I have seen the bilateral interstitial pneumonia on the xray of the asymptomatic shoulder dislocation or on the CT's of the (respiratory) asymptomatic polytrauma patient. Essentially if they are in my ER, they have it. Seen three positive flu swabs in 2 weeks and all three had Covid 19 as well. Somehow this ***** has told all other disease processes to get out of town.
China reported 15% cardiac involvement. I have seen covid 19 patients present with myocarditis, pericarditis, new onset CHF (
Congestive heart failure) and new onset atrial fibrillation. I still order a troponin, but no cardiologist will treat no matter what the number in a suspected Covid 19 patient. Even our non covid 19 STEMIs (
ST-Elevation Myocardial Infarction; serious heart attack) at all of our facilities are getting TPA (
Tissue plasminogen activator used to dissolve blood clots) in the ED (
Emergency Department) and rescue PCI (
Percutaneous Coronary Intervention; aka angioplasty with stint) at 60 minutes only if TPA fails.
Diagnostic CXR (
Chest X-Ray)- bilateral interstitial pneumonia (anecdotally starts most often in the RLL (
lower lobe of the right lung) so bilateral on CXR is not required). The hypoxia does not correlate with the CXR findings. Their lungs do not sound bad. Keep your stethoscope in your pocket and evaluate with your eyes and pulse ox.
Labs- WBC (
white blood cell count) low, Lymphocytes low, platelets lower than their normal, Procalcitonin (
substance produced in response to bacterial infections but also in response to tissue injury) normal in 95%.
CRP (
C-Reactive Protein Test: A plasma protein that rises in the blood with the inflammation from certain conditions) and Ferritin (
blood protein that indicates iron level) elevated most often. CPK (
creatine phosphokinase: elevated levels indicate muscle trauma, including heart), D-Dimer (
a small protein fragment present in the blood after a blood clot is degraded by fibrinolysis), LDH (
Lactate dehydrogenase: plays an important role in cellular respiration, the process by which glucose (sugar) from food is converted into usable energy for our cells.), Alk (
Anaplastic lymphoma kinase: plays a pivotal role in cellular communication and in the normal development and function of the nervous system), Phos (
Phosphorus level: key to kidney function)/AST (
Aspartate aminotransferase: released into blood when the liver or heart is damaged)/ALT (
alanine transaminase: high levels can indicate a liver problem) commonly elevated.
Notice D-Dimer- I would be very careful about CT PE (
CT pulmonary angiography used to detect pulmonary embolisms) these patients for their hypoxia. The patients receiving IV contrast are going into renal (
kidney) failure and on the vent sooner.
Basically, if you have a bilateral pneumonia with normal to low WBC, lymphopenia, normal procalcitonin, elevated CRP and ferritin- you have covid-19 and do not need a nasal swab to tell you that.
A ratio of absolute neutrophil (
type of white blood cell) count to absolute lymphocyte (
type of white blood cell) count greater than 3.5 may be the highest predictor of poor outcome. the UK is automatically intubating these patients for expected outcomes regardless of their clinical presentation.
An elevated Interleukin-6 (
IL6: stimulates the inflammatory and auto-immune processes in many diseases) is an indicator of their cytokine storm. If this is elevated watch these patients closely with both eyes.
Other factors that appear to be predictive of poor outcomes are thrombocytopenia (
low blood platelet count) and LFTs
(liver function test) 5x upper limit of normal.
DispositionI had never discharged multifocal pneumonia before. Now I personally do it 12-15 times a shift. 2 weeks ago we were admitting anyone who needed supplemental oxygen. Now we are discharging with oxygen if the patient is comfortable and oxygenating above 92% on nasal cannula. We have contracted with a company that sends a paramedic to their home twice daily to check on them and record a pulse ox. We know many of these patients will bounce back but if it saves a bed for a day we have accomplished something. Obviously we are fearful some won't make it back.
We are a small community hospital. Our 22 bed ICU and now a 4 bed Endoscopy suite are all Covid 19. All of these patients are intubated except one. 75% of our floor beds have been cohorted into covid 19 wards and are full. We are averaging 4 rescue intubations a day on the floor. We now have 9 vented patients in our ER transferred down from the floor after intubation.
Luckily we are part of a larger hospital group. Our main teaching hospital repurposed space to open 50 new Covid 19 ICU beds this past Sunday so these numbers are with significant decompression. Today those 50 beds are full. They are opening 30 more by Friday. But even with the "lockdown", our AI models are expecting a 200-400% increase in covid 19 patients by 4/4/2020.
TreatmentSupportive
worldwide 86% of covid 19 patients that go on a vent die. Seattle reporting 70%. Our hospital has had 5 deaths and one patient who was extubated. Extubation happens on day 10 per the Chinese and day 11 per Seattle.
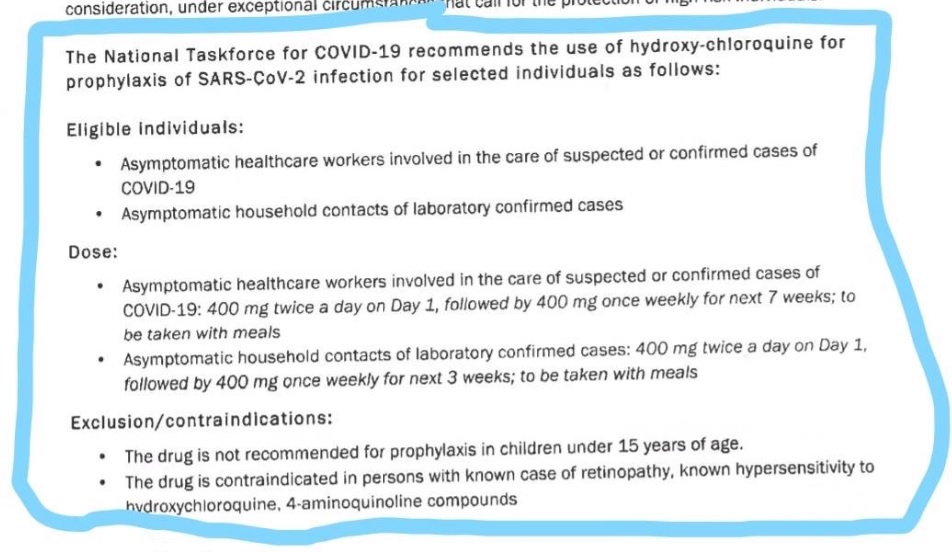
Plaquenil which has weak ACE2 (
angiotensin-converting enzyme) blockade doesn't appear to be a savior of any kind in our patient population. Theoretically, it may have some prophylactic properties but so far it is difficult to see the benefit to our hospitalized patients, but we are using it and the studies will tell. With Plaquenil's potential QT prolongation (
refers to an interval seen in an electrocardiogram (EKG) test of heart function) and liver toxic effects (both particularly problematic in covid 19 patients), I am not longer selectively prescribing this medication as I stated on a previous post.
We are also using Azithromycin, but are intermittently running out of IV.
Do not give these patient's standard sepsis fluid resuscitation. Be very judicious with the fluids as it hastens their respiratory decompensation. Outside the DKA and renal failure dehydration, leave them dry.
Proning vented patients significantly helps oxygenation. Even self proning the ones on nasal cannula helps.
Vent settings- Usual ARDS stuff, low volume, permissive hypercapnia, etc. Except for Peep of 5 will not do. Start at 14 and you may go up to 25 if needed.
Do not use Bipap (
Bilevel Positive Airway Pressure, and is very similar in function and design to a CPAP machine )- it does not work well and is a significant exposure risk with high levels of aerosolized virus to you and your staff. Even after a cough or sneeze this virus can aerosolize up to 3 hours.
The same goes for nebulizer treatments. Use MDI. you can give 8-10 puffs at one time of an albuterol MDI (
Metered-dose inhaler). Use only if wheezing which isn't often with covid 19. If you have to give a nebulizer must be in a negative pressure room; and if you can, instruct the patient on how to start it after you leave the room.
Do not use steroids, it makes this worse. Push out to your urgent cares to stop their usual practice of steroid shots for their URI (
upper respiratory infection)/bronchitis.
We are currently out of Versed, Fentanyl, and intermittently Propofol. Get the dosing of Precedex and Nimbex back in your heads.
One of my colleagues who is a 31 yo old female who graduated residency last may with no health problems and normal BMI is out with the symptoms and an SaO2
(saturated O2 level in the blood) of 92%. She will be the first of many.
I PPE best I have. I do wear a MaxAir PAPR the entire shift. I do not take it off to eat or drink during the shift. I undress in the garage and go straight to the shower. My wife and kids fled to her parents outside Hattiesburg. The stress and exposure at work coupled with the isolation at home is trying. But everyone is going through something right now. Everyone is scared; patients and employees. But we are the leaders of that emergency room. Be nice to your nurses and staff. Show by example how to tackle this crisis head on. Good luck to us all.